Recent News
- RadiomixNet for Advanced Pneumonia Diagnosis February 27, 2025
The research team from the Department of Electronics and Communication Engineering has published a paper titled “RadiomixNet: Integrating Radiomics and Feature Extraction for Advanced Pneumonia Diagnosis” in the journal IEEE Access with an impact factor of 3.4. Prof. Siva Sankar Yellampalli, Professor of Practice, and Mr Rahul Gowtham, PhD Scholar, have worked on RadiomixNet, a smart computer-assisted system designed to help doctors diagnose pneumonia more accurately using chest X-ray images.
Abstract
The research presents RadiomixNet, a pneumonia diagnosis framework integrating radiomics-based feature extraction with advanced classification techniques. Chest X-ray images are pre-processed using denoising, resizing, and enhancement methods to ensure uniformity and high image quality. Radiomics features are extracted using Gray Level Co-Occurrence Matrix (GLCM), Gray Level Size Zone Matrix (GLSZM), Gray Level Run Length Matrix (GLRLM), and Gray Level Dependence Matrix (GLDM). Power Spectral Density (PSD) analysis using Burg, Yule Walker, and Welch techniques enhances the understanding of frequency characteristics within the radiomics feature matrices. To classify pneumonia cases, machine learning classifiers such as Bernoulli Naïve Bayes, Random Subspace Boost, Quadratic Discriminant, and Gradient Boosting are employed. Among these, Gradient Boosting demonstrated superior performance, achieving a Cohen’s Kappa of 0.93, MCC of 0.88, Youden’s Index of 0.82, and a Log Loss of 0.27. The proposed methodology enhances diagnostic accuracy, reduces variability in pneumonia detection, and provides a structured approach to feature-based pneumonia classification.
Explanation of the Research in Layperson’s Terms
Traditional diagnosis relies on a doctor visually examining the X-ray, which can sometimes lead to misinterpretations. RadiomixNet improves this process by using advanced image processing and artificial intelligence (AI) techniques.
- Preprocessing the X-rays – Before analysis, we clean the images by removing noise (unwanted distortions), adjusting brightness, and resizing them to a standard format. This ensures all images are high quality and uniform.
- Generating More Training Data – Since AI models need a large amount of data to learn effectively, we use Generative Adversarial Networks (GANs) to create additional synthetic X-ray images. This helps balance the dataset and improve the model’s ability to detect pneumonia accurately.
- Extracting Hidden Patterns – The system breaks down X-ray images into tiny texture and shape details using advanced techniques like GLCM, GLSZM, GLRLM, and GLDM. These methods capture the structure of the lungs and highlight patterns that indicate pneumonia.
- Analysing Frequency Components – Similar to how an audio equalizer separates different sound frequencies, we analyze the X-ray’s frequency components using techniques like Burg PSD, Yule Walker PSD, and Welch PSD. This helps uncover hidden details in the images that may not be visible to the human eye.
- Making the Final Diagnosis – After extracting these detailed features, we use AI models to classify the images as “pneumonia” or “healthy.” We tested different models, including Naïve Bayes, Random Subspace Boost, Quadratic Discriminant, and Gradient Boosting. Among them, Gradient Boosting performed the best, making the most accurate predictions.
- Evaluating Accuracy – To ensure the system is reliable, we used various accuracy-checking methods such as Cohen’s Kappa, Matthews Correlation Coefficient (MCC), Sensitivity, Specificity, Log Loss, and Brier Score.
Practical Implementation/Social Implications of the Research
Practical Implementation:
RadiomixNet has the potential to be integrated into real-world healthcare systems to assist in pneumonia diagnosis. Its implementation can take place in various ways:
- Hospital Integration – RadiomixNet can be deployed in hospitals as a decision-support tool for radiologists. By analysing chest X-rays in real time, it can provide secondary validation, reducing diagnostic errors and improving accuracy in pneumonia detection.
- Telemedicine and Remote Diagnosis – The system can be integrated into telemedicine platforms, allowing doctors in rural or under-resourced areas to diagnose pneumonia remotely. Patients can upload their X-ray images, and RadiomixNet can assist in providing a preliminary diagnosis.
- Medical Imaging Centers – Radiology centers can incorporate RadiomixNet into their existing Picture Archiving and Communication Systems (PACS) to enhance diagnostic efficiency, reduce the workload of radiologists, and provide automated analysis.
- Edge Computing in Low-Resource Settings – Unlike deep learning models that require expensive GPUs, RadiomixNet is optimized for standard computing hardware. This makes it feasible for implementation in clinics and hospitals that lack high-end computational resources.
- Clinical Trials and Further Validation – Pilot studies in hospitals can validate RadiomixNet’s accuracy and reliability before widespread deployment. The system can be fine-tuned based on real-world patient data to improve its performance across diverse populations.
Social Implications:
- Early and Accurate Diagnosis – By improving pneumonia detection, RadiomixNet can enable earlier treatment, reducing complications and mortality rates, especially in high-risk populations such as children, the elderly, and immunocompromised individuals.
- Reducing Radiologist Workload – With increasing patient loads, radiologists often face diagnostic fatigue. RadiomixNet can act as an assistant, helping them focus on complex cases while automating routine pneumonia detection.
- Bridging the Healthcare Gap – In developing countries where expert radiologists are scarce, RadiomixNet can assist general practitioners and healthcare workers in diagnosing pneumonia without requiring extensive radiology expertise.
- Affordable and Scalable Solution – Since the system does not require expensive hardware, it can be implemented in low-resource settings, making advanced pneumonia detection accessible to a broader population.
- Pandemic Preparedness – Pneumonia is a major complication of respiratory infections like COVID-19. RadiomixNet can be adapted to detect pneumonia-related lung infections, aiding in large-scale screening during outbreaks.
By integrating RadiomixNet into healthcare systems, we can enhance diagnostic accuracy, improve patient outcomes, and make pneumonia diagnosis more accessible and efficient globally.
Continue reading →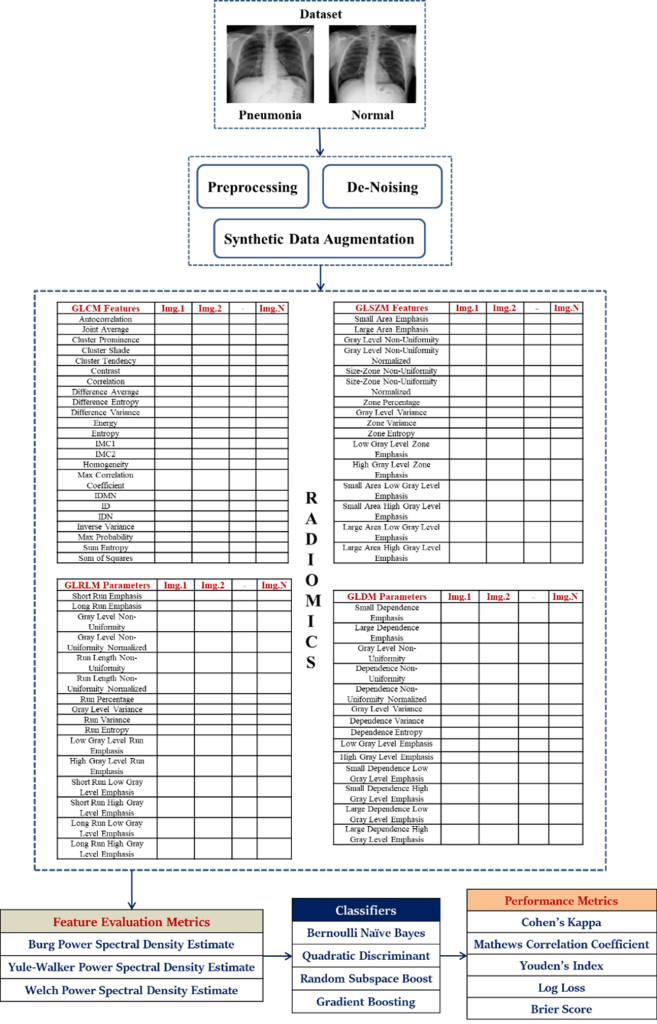
RadiomixNet Implementation Framework
- Patent on Pneumonia Diagnosis Using Deep Learning Techniques February 27, 2025
 In the patent titled “A System and a Method For Real-Time Pneumonia Diagnosis On a Resource- Constrained Hardware Platform,” authored by Prof. Siva Sankar Yellampalli from the Department of ECE and his research scholars – Mr Rahul Gowtham Poola and P L Lahari, a novel diagnostic solution is presented to enhance pneumonia detection in low-resource settings. With Application No: 202441084727, this research explores the integration of advanced deep learning techniques with a compact microcontroller-based system, providing an innovative approach to improve healthcare accessibility and prompt medical intervention.
In the patent titled “A System and a Method For Real-Time Pneumonia Diagnosis On a Resource- Constrained Hardware Platform,” authored by Prof. Siva Sankar Yellampalli from the Department of ECE and his research scholars – Mr Rahul Gowtham Poola and P L Lahari, a novel diagnostic solution is presented to enhance pneumonia detection in low-resource settings. With Application No: 202441084727, this research explores the integration of advanced deep learning techniques with a compact microcontroller-based system, providing an innovative approach to improve healthcare accessibility and prompt medical intervention.Abstract:
The research focuses on the development of an innovative system for real-time pneumonia diagnosis leveraging advanced deep learning techniques integrated with edge computing technology. The proposed solution employs the MAX78000 microcontroller, a resource-constrained hardware platform, to deploy a sophisticated neural network model capable of analyzing chest X-ray images. The invention addresses the pressing need for accessible, cost-effective, and efficient diagnostic tools in under-resourced and remote environments. The system encompasses a complete diagnostic pipeline, including image acquisition via an onboard parallel camera module, real-time image processing, and display of results on a 3.5″ touch-enabled TFT screen. The deep learning model, optimized for the constraints of the MAX78000, performs real-time classification of chest X-ray images into either normal or pneumonia-affected categories. By operating entirely on-device, the system eliminates the need for high-power servers or internet connectivity, thereby reducing latency and dependency on external infrastructure. This research emphasizes portability, energy efficiency, and low-cost deployment, making the solution highly suitable for primary healthcare facilities, rural clinics, mobile health units, and disaster-response scenarios. With the ability to deliver immediate, accurate diagnoses, the device significantly enhances clinical decision-making and enables timely medical intervention. Additionally, the scalable and adaptable design of the system opens possibilities for broader medical imaging applications, extending its utility beyond pneumonia diagnostics. Experimental results showcase the performance of the neural network model, demonstrating prediction accuracies ranging between 66% and 97% for different test cases on the MAX78000 microcontroller. These findings underline the potential of the proposed system as a transformative tool for advancing point-of-care diagnostics in low-resource settings.
Explanation in Layperson’s terms.
The research presents a compact, affordable device that helps doctors quickly detect pneumonia by analyzing chest X-ray images in real-time. It uses advanced artificial intelligence (AI) technology, called deep learning, to examine the X-rays and determine whether a patient has pneumonia or not. What makes this device special is that it works entirely on a small, low-power microcontroller called the MAX78000, instead of needing powerful computers or internet access. The process begins when the device captures a chest X-ray image using its built-in camera. Then, the AI model, which has been trained to recognize patterns associated with pneumonia, analyzes the image. The results are displayed instantly on a small screen, allowing healthcare providers to make quick decisions. This real-time diagnosis can be life-saving, especially in emergency or rural settings where access to advanced medical equipment or high-speed internet is limited. Technically, this system combines AI and edge computing, meaning all the heavy processing happens directly on the device rather than in remote servers. This design keeps costs low, ensures patient data privacy, and makes the device highly portable and energy-efficient. The technology can work even in places with unreliable electricity, making it ideal for use in mobile health units, rural clinics, or disaster zones. Additionally, the invention can be adapted for diagnosing other diseases, showcasing its versatility in improving healthcare globally.
Practical Implementation
This research can be practically implemented as a compact, standalone device for diagnosing pneumonia in healthcare settings where access to advanced medical equipment is limited. It works as follows:
- Deployment in Rural Clinics and Mobile Health Units: The device can be used in clinics in remote or underserved areas where large X-ray machines and advanced computing resources are unavailable. It provides on-the-spot diagnosis.
- Point-of-Care Diagnostics: The portability and integration of image acquisition, AI-based processing, and display into a single unit make it ideal for bedside use in hospitals or during emergency care.
- Disaster Response: Its low-power and internet-free design make it a critical tool in disaster zones, refugee camps, or any setting where power and connectivity are unreliable.
- Telemedicine Integration: The device can complement telemedicine by providing accurate diagnostic results to remote doctors, helping bridge the gap between frontline healthcare workers and specialists.
Social Implications
Improved Access to Healthcare: By making pneumonia diagnosis accessible in rural and underserved regions, this device can drastically reduce the gap in healthcare services between urban and remote areas. It empowers healthcare providers in low-resource settings to deliver timely diagnoses.
- Affordability: The use of a low-cost microcontroller ensures that the device is affordable for governments and healthcare organizations, particularly in developing countries. This can enhance healthcare access for low-income populations.
- Reduced Mortality Rates: Pneumonia is a leading cause of death in children under five and elderly individuals, especially in low-income countries. This device’s ability to provide real-time, accurate diagnosis allows for earlier intervention and treatment, potentially saving countless lives.
- Privacy and Security: Since all data is processed locally on the device, it ensures patient privacy by eliminating the need to transfer sensitive medical data to cloud servers, addressing concerns about data security.
- Scalability: The underlying technology can be adapted to diagnose other diseases, creating a broader impact on global health. For example, similar systems could be used for tuberculosis, COVID-19, or other respiratory conditions, further enhancing healthcare infrastructure.
By addressing critical gaps in diagnostic capabilities and ensuring accessibility and affordability, this research has the potential to transform healthcare delivery and improve quality of life, especially in marginalized communities.
Collaborations:
Rahul Gowtham Poola, Ph.D Scholar, Dept of ECE, SRM University-AP
P.L. Lahari, Ph.D Scholar, Dept of ECE, SRM University-AP
Prof. Siva Sankar Yellampalli, Professor of Practice, Dept of ECE, SRM University-AP
- Collaboration with Sibar to Boost Research Advancements February 27, 2025
 SRM University-AP formalised a significant Memorandum of Understanding (MoU) with the Sibar Institute of Dental Sciences, Guntur. The MoU is aimed at advancing the field of Biomedical Engineering & Biomedical Sciences and leverage SRM University-AP’s technical expertise alongside the medical proficiency of Sibar Institute, to foster groundbreaking innovations.
SRM University-AP formalised a significant Memorandum of Understanding (MoU) with the Sibar Institute of Dental Sciences, Guntur. The MoU is aimed at advancing the field of Biomedical Engineering & Biomedical Sciences and leverage SRM University-AP’s technical expertise alongside the medical proficiency of Sibar Institute, to foster groundbreaking innovations.The MoU was signed in a ceremony by Principal, Dr B Venkat Ramana Reddy from Sibar Institute of Dental Sciences and Registrar, Dr R Premkumar from SRM University-AP. Notable attendees included Vice Chancellor, Prof. Manoj K Arora, Dean-SEAS Prof. C V Tomy; Dean-Research Prof. Ranjit Thapa; Head of the Department of ECE, Dr K A Sunitha; Chief Medical Officer, Dr Raju Dudam from the SRM AP Medical Centre, alongside faculty from the Departments of Computer Science and Engineering, Electronics and Communication Engineering, Biological Sciences and Chemistry and medical practitioners from Sibar Institute of Dental Sciences including Dean, Dr L Krishna Prasad; Dr K Kiran Kumar, Prof and Head, Department of Oral Pathology; Dr P Chandrashekhar, Professor- Department of Pathology and Dr D Ravinath Professor & Head, Department of Peridontics.
During the event, Vice Chancellor Prof. Manoj K. Arora pointed out the university’s rapid growth in both research and academic realms. He highlighted SRM AP‘s collaborations with esteemed institutions abroad stressing on the varsity’s commitment to interdisciplinary learning and research. Prof. Arora stated, “By merging engineering brilliance with medical sciences, we aim to achieve breakthroughs that will significantly benefit the society.”
Registrar Dr R Premkumar articulated the university’s dedication to research and its mission to bring transformational change. He remarked, “Our Faculty is our greatest asset, and we are prepared to extend all support to foster a transformative change in the society.”
Discussions from Dean-Research Prof. Ranjit Thapa, Dean-SEAS Prof. C V Tomy, and Associate Dean ( Admission Outreach and Research Collaborations), Prof. Jayaseelan Murugaiyan, on the collaborative research opportunities and clinical studies between the two institutions added significant value to the partnership.
Dean, Dr L Krishna Prasad from Sibar Institute of Dental Sciences expressed his enthusiasm in partnering with SRM AP and looked forward to this collaborative engagement to make significant breakthrough in the field of medical sciences and research.
Dr K A Sunitha highlighted the potential for knowledge exchange through this partnership, noting plans for joint data collection and analysis. The collaboration will extend to community welfare too, wherein dental health camps in the six villages adopted by SRM AP will be offered.
- Developing Organic Thin-Film Transistors into Biosensors February 17, 2025
The Department of Electronics and Communication Engineering is proud to announce that Dr Durga Prakash M and his scholar Prasanthi Ms Prasanthi Lingala have their invention titled “An Organic Thin-Film Transistors (OTFTs) with Steep Subthreshold and Ultra-Low Temperature Solution Processing for Label-Free Biosensing” published in the Indian Patent Office Journal with the Application Number: 202541000088. Their research focus on developing an Organic Thin-Film Transistor (OTFT) that is able to work as a biosensor in detecting diseases or for real-time health monitoring.
Abstract
Organic Thin-Film Transistor (OTFT): The name “organic thin-film transistor” (OTFT) refers to a type of transistor that employs organic semiconductor materials in its active layer rather than the more traditional inorganic materials such as silicon. Optical thin-film transistors (OTFTs) are distinguished by their adaptability, low fabrication cost, and optimal applicability for electronic devices that are lightweight and portable. Considering their high sensitivity to changes in the surrounding environment and their compatibility with functionalised layers for the detection of biomolecules, these transistors find widespread application in the field of biosensors.
Explanation of the Research in Layperson’s Terms
Imagine a flexible electronic switch that can be bent, stretched, and used in lightweight devices—this is what an Organic Thin-Film Transistor (OTFT) does! Unlike traditional transistors made from rigid silicon, OTFTs use special organic materials, making them more adaptable for wearable sensors, flexible displays, and medical devices.
The research focuses on how these transistors can be used as biosensors, meaning they can detect tiny changes in the environment, like the presence of certain chemicals or biomolecules. This is important for medical testing, where OTFTs could help develop low-cost, highly sensitive diagnostic tools—imagine a simple patch that can detect diseases from sweat or a flexible sensor for real-time health monitoring! By improving how OTFTs interact with biological substances, the team aims to make them more accurate, efficient, and reliable for next-generation healthcare and wearable technology.
Continue reading →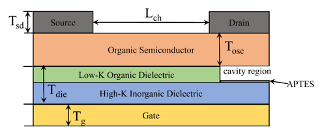
Fig.: Schematic structure of DNTT based OTFT
- A Novel System for Breast Cancer Diagnosis January 29, 2025

Faculty duo from the Department of Electronics and Communication Engineering, Dr Anirban Ghosh and Dr Sunil Chinnadurai, along with their research cohort, Phanindra Rayapudi Venkata, Baswala Srujana, Gadde Saranya, and Abburi Sowgandhi (B.Tech. ECE students) have published their patent titled “A System and Method for Breast Cancer Diagnosis” (Application number: 202441088356). Their cutting-edge research presents a system to help diagnose breast cancer more accurately and efficiently using advanced image analysis techniques.
Abstract
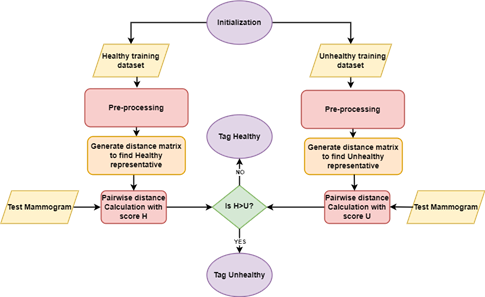
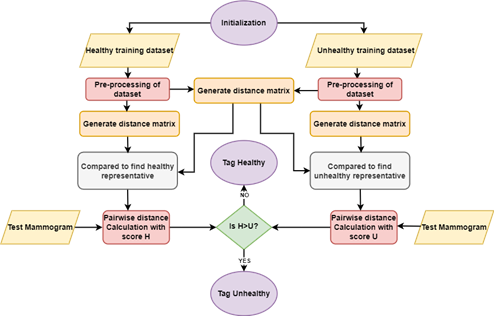
The present disclosure discloses a system for diagnosing breast cancer that utilizes topological data analysis to transform mammogram images into meaningful diagnostic insights. It includes a data preprocessing module for image standardization and enhancement and a feature extraction module to create histograms for topological analysis. The topological data analysis module converts these histograms into Persistent Homology Diagrams (PHDs) representing topological features. An Earth Mover’s Distance (EMD) matrix is generated by a similarity metric module to compare PHDs. Representative PHDs are identified using a representative selection module, enabling accurate classification by the classification module. The system’s performance is assessed through various metrics by a performance analysis module, and a web service module provides an intuitive interface for users to upload images and receive diagnostic results. This approach enhances breast cancer detection by focusing on persistent topological features, offering improved precision and interpretability.
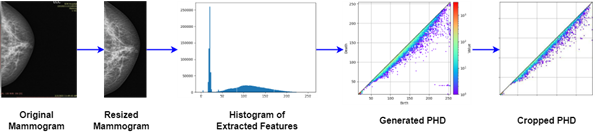
Figure 1. Conversion of mammograms into PHDs
Explanation of the Research in Layperson’s Terms
Here’s how the system works in simple terms:
1. Preparing the Images: Mammogram images are cleaned and adjusted to ensure they’re clear and easy to analyse. The focus is on areas that might show signs of cancer.
2. Extracting Patterns: The system looks for patterns in the images that could indicate healthy or unhealthy tissue. It turns these patterns into a visual map that represents the shape and structure of the tissue.
3. Analysing Shapes: The system uses math to study how these shapes appear and disappear as the image details change. The most persistent shapes (important ones) are kept, and random noise is ignored.
4. Comparing Images: A tool measures how similar or different these patterns are between images. This helps the system group them into healthy or cancerous categories.
5. Making a Decision: The system compares a new mammogram to its library of known patterns to decide whether it’s likely healthy or shows signs of cancer.
6. Easy to Use: Doctors can upload an image to a web-based tool and quickly get results, complete with visual explanations.
This system helps doctors by making the diagnosis process faster, more reliable, and easier to understand, which can lead to earlier and better treatment for breast cancer.
Practical Implementation/Social Implications of the Research
This research enhances breast cancer detection by enabling earlier, more accurate diagnoses and improving survival rates. Its web-based tool ensures access to advanced diagnostics in remote and underserved areas, reducing disparities in healthcare. Supporting radiologists with objective insights minimizes errors and workload, especially in resource-limited settings. Patients benefit from faster, clearer results, leading to timely and cost-effective treatment. Additionally, the innovative methods could inspire advancements in diagnosing other diseases, driving broader medical progress and improving global health outcomes.
Future Research Plans
Future research could expand this system to detect other diseases like lung or liver cancer, improve diagnostic accuracy by reducing false results, and integrate multimodal data for comprehensive analysis. Incorporating patient-specific information for personalized risk assessments, creating self-learning models, and optimizing computational efficiency could enhance its adaptability. Large-scale global trials and user-friendly interfaces would ensure effective implementation across diverse populations and healthcare systems, making the technology more versatile, accessible, and impactful.
Continue reading →